Asthma
Asthma (or Asthma bronchiale) is a disease that hurts the airways inside the lungs. It causes the tissue inside the airways to swell. Asthma also causes the bands of muscle around the airways to become narrow. This makes it hard for enough air to pass through and for the person to breathe normally. Asthma also causes mucus-making cells inside the airways to make more mucus than normal. This blocks the airways, which are already very narrow during an asthma attack, and makes it even more difficult to breathe.
| Asthma | |
|---|---|
| Classification and external resources | |
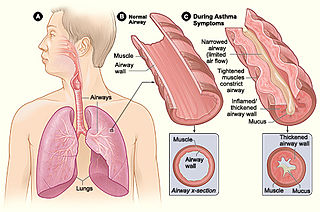 An asthma attack causes the airways to get smaller and too much mucus to be made. This makes it hard to breathe. | |
| ICD-10 | J45. |
| ICD-9 | 493 |
| OMIM | 600807 |
| DiseasesDB | 1006 |
| MedlinePlus | 000141 |
| eMedicine | article/806890 |
| MeSH | D001249 |
A person having an asthma attack often makes wheezing sounds when trying to breathe. This is the sound of air trying to pass through the very narrow airway. They also have shortness of breath, which means they cannot take a full deep breath. Chest tightness may happen which feels like their chest is being squeezed. They may also cough a lot.
Asthma attacks can be a medical emergency because they can be fatal (cause a person to die). There is no cure for asthma. There are treatments such as different kinds of medicines to help people with asthma. There are also things that people with asthma can do to help themselves to keep their asthma from getting worse.
There are a lot of risk factors for getting asthma. The exact reasons for each is not yet clearly understood. Some of the factors are believed to come from genetics. A person inherits genetic mutations from one or both of their parents that may increase the chances of developing asthma. Epigenetics, which are changes in the way a gene acts, may also increase their chances of getting asthma. These epigenetic changes may also be inherited. They may happen when a baby is still growing inside its mother, or during childhood.
Socioeconomic status (SES) is also believed to play a part in developing asthma. A person's socioeconomic status is based on such things as how much money their family makes, where they live, and their education level. Race and ethnicity also may play a part. It also is related to access to medical care, personal beliefs, and dietary habits. People of lower socioeconomic status suffer higher rates of asthma, have worse outcomes, and also have higher asthma-related death rates than people of higher economic status.
Causes
The exact cause of asthma is not yet known. It is believed that it may be because of a of many different reasons:
Genetics: When changes happen in a person's genes (called mutations) these changes are passed on to their children. One or both parents may have these changes or mutations in their genes, and some or all of their children may be born with them, which means they inherited them. These mutations, once they happen, run in families from one generation to the next and are permanent mutations, they change the gene in the DNA. These changes can make a person more likely to get certain diseases like asthma. In some diseases it may be only one change in one gene that may make a person get that disease, in asthma it may be changes in many different genes that may make a person more likely to get asthma.[1]
Epigenetics changes or modifications cause different kind of changes that affect how a person's genes work or 'express themselves' in three different ways (called epigenetic mechanisms), but do not change the gene in the DNA. These epigenetic changes may be inherited, or they may happen in utero which is when a baby is still inside its mother. They may also happen in childhood, because of different reasons, like a respiratory infection, being exposed to chemicals or drugs, diet etc. These changes can be passed from one generation to the next but are not permanent and might only be passed down one or two generations. Even though epigenetic changes affect how a person's genes work they do not permanently change a person's genes. It is believed epigenetic changes may also make a person more likely to get certain diseases like asthma.[2]
Environmental factors are things that affect a person; which can be either healthy or unhealthy. Unhealthy environmental factors are things like living in an area where there is a lot of air pollution, or living somewhere where there are lots of bugs in the house, or being around cigarette smoke.
If a person who has genetic or epigentic changes in their genes that makes them have a bigger chance of getting asthma (genetic predisposition), also has unhealthy environmental factors in their life, like living in a home that has a lot of dust mites, then it is more likely that they will get asthma.
Atopy
Atopy is when there are changes in some of the genes a person is born with (genetic inheritance). These genetic changes make their body produce more Immunoglobulin E (IgE), a type of antibody. They are also more sensitive to things things like chemicals, smoke and dust (environmental antigens). This hypersensitivity means they are more sensitive or allergic to things in the environment than people who do not have these changes in their genes and are not hypersensitive or allergic.
This hypersensitivity causes their body to react in certain ways. Usually a person who is atopic develops allergic rhinitis which affects the nasal passages which are behind the nose and they are also more likely to get atopic dermatitis which causes skin rashes and atopic asthma. Up to 40% of people with allergic rhinitis also have asthma.[3] These three medical problems, allergic rhinitis, atopic dermatitis and atopic asthma are called the Atopic Triad (a triad is when there is three of something).[4] People who are atopic may also have other medical problems including food and drug allergies, stinging-insect hypersensitivity, hives (urticaria), Quincke's edema (angioedema), and contact dermatitis.
If a person has one parent who is atopic they have a chance of being atopic too. If they have two parents who are atopic they have an even bigger chance of being atopic.[5]
Acetaminophen and asthma
There have been studies that show a link between acetaminophen (Tylenol) and asthma. For instance a 2008 analysis of information collected from a very large study called the International Study of Asthma and Allergies in Childhood, or the "Isaac study" for short, showed that children who had taken acetaminophen for a fever during the first year of their life had a 50% higher risk of getting asthma later on.[6] The more acetaminophen children took the higher their risk of getting asthma. Children who took it once a month had threefold increase in their risk of getting asthma. An increase in asthma rates in multiple countries corresponded with increased sales of drugs which contained acetaminophen.[7][8] Previously the American College of Physicians reported a link between non-atopic asthma and acetaminophen use based on results of The Third National Health and Nutrition Examination Survey.[9] Not all doctors are convinced of the link between acetaminophen and asthma.
"Children with asthma or at risk for asthma should avoid the use of acetaminophen." (McBride JT, 2011[10]).
Types of Asthma
Atopic asthma
Atopic asthma is the most common form of asthma.
Cough-variant asthma
Cough-variant asthma is a type of asthma in which a cough is the main, and sometimes only sign. Cough-variant asthma usually does not cause wheezing or breathlessness and causes a dry, scratchy, mostly nonproductive cough (this means little or no phlegm is coughed up). About 30% of people who have cough-variant asthma will develop typical asthma.[13]
Work-related asthma
Work related asthma are types of asthma that are caused or made worse by irritants in the environment at a person's place of work. The kind of jobs that may cause work related asthma are usually those in which there is a lot of smoke or chemicals are used. There are different types of work-related asthma (WRA):[14]
1. Occupational asthma with latency: this asthma type is when the signs and symptoms of asthma occur after a period of time (latency) after being exposed to the environmental irritants. e.g.: John starts working at a factory where chemicals are used the first week of January. At the end of March he starts developing the signs and symptoms of asthma. The period of time from when he started the job in January to when the signs and symptoms of asthma started in March is the latency period.[15]
2. Irritant-Induced Asthma (IIA) is occupational asthma without latency: this is an asthma type is when the signs and symptoms of asthma can occur immediately (without latency) after being exposed to the environmental irritants. e.g. Frank starts a new job working as a janitor where he uses ammonia to clean. After opening the bottle of ammonia and breathing the fumes Frank starts finding it difficult to breath, his chest tightens up and he develops other signs and symptoms of asthma.[16]
- 3. Reactive Airways Dysfunction Syndrome (RADS):
4. Work-aggravated asthma: this is when a person already has asthma and environmental triggers at their place of work makes it worse.
Exercise induced asthma
Exercise induced asthma (EIA) - also called exercise induced bronchospasm - is the term used to describe asthma cases in which exercise is the main, and many times the only trigger for an asthma attack. If a person already has a form of asthma or they are atopic there is more of a chance of getting EIA.
Nocturnal asthma
Nocturnal asthma: is the term used to describe asthma cases that get worse at night (nocturnal).
Premenstrual asthma (PMA): is when asthma symptoms get worse during the premenstrual period. This condition may affect up to 40% of female asthma sufferers. For a diagnosis of PMA to be made it is necessary to have a detailed history of the timing of menstrual cycles along with asthma symptoms experienced, and the peak expiratory flow rate (PMA may cause the PEF to be lowered in the premenstrual period). It is helpful in making a diagnosis to keep a diary of symptoms and peak expiratory flow (PEF) rates.[17][18]
Status asthmaticus
Status asthmaticus is a severe form of asthma in which an asthma attack gets worse as it goes along and the medicines that are usually used to treat asthma do not work. Status asthmaticus can be fatal.[19]
Signs and symptoms
| |||||
| Problems listening to this file? See media help. | |||||
Signs and symptoms in medicine are the way a medical condition affects a person's body. Sometimes the signs and symptoms of asthma may be mild which does not bother the person too much. At other times they may be severe which may make the person feel very sick.
Not every person with asthma has all the signs and symptoms of asthma all the time. A person may have some signs and symptoms during one asthma attack and have different symptoms during another asthma attack. Some people with asthma may have long periods of time between asthma attacks where they show no signs and experience no symptoms of asthma, while others may have some or all of the signs and symptoms everyday which become more severe during an attack. It also depends on what type of asthma a person has and whether they have a mild, moderate or severe case.
There are also some people with asthma who might only have signs and symptoms during certain times, such as those with exercise induced asthma, where the exercise triggers the symptoms. For some the signs and symptoms of asthma may be triggered or made worse (exacerbated) when they have viral respiratory tract infections, often the type casued by human rhinoviruses.[20]
Early warning signs of an asthma attack are physical changes in health that a person with asthma has before they have the attack. By knowing the early warning signs a person may be able to take steps to keep from having an asthma attack or if they do have one, to keep it from getting worse.
Early warning signs
The early warning signs of asthma may include:
- Coughing a lot, especially at night
- Losing your breath easily
- Shortness of breath: this is when a person cannot take a deep breath which means they cannot fill their lungs all the way with air. They may be only able to take short, shallow breaths which does give their lungs enough air. When a person has shortness of breath they may also have chest tightness.
- Getting tired easily during exercise and feeling weak and wheezing or coughing after exercise
- Feeling the symptoms of a cold or allergies coming on like sneezing, a runny or stuffed up nose, coughing, sore throat, and headache
Triggers
A trigger factor or trigger for short, is something that causes the signs and symptoms of a medical condition to begin in a person who already has that medical condition. Common triggers for asthma are:
- Tobacco smoke: a person does not need to smoke themselves, second-hand smoke can trigger an asthma attack. Second-hand smoke is the smoke from the end of a burning cigarette, cigar or pipe that someone else is smoking, or the smoke that they breathe out (exhale).
- Pets: animals give off chemicals called proteins which are allergens; people can be allergic to them. These allergens can act as irritants and make someone's asthma worse and trigger an asthma attack. The proteins are in the pet's dander which is the dead flakes of skin that animals (and people) shed. They are also in their urine, feces, saliva, and sebum which is made by glands in the skin called sebaceous glands. Sebum is what makes hair and skin oily. When dander, urine, feces, saliva, and sebum dry out their proteins can become airborne and breathed in. Some of the types of pets people can be allergic to are, dogs, cats, gerbils, hamsters, guinea pigs and pet birds.
- Bugs: different types of bugs which may be found inside homes may trigger asthma attacks. They may trigger asthma symptoms in the same way as pets; the proteins they give off are allergens and become airborne. Some of the more common bugs which may trigger asthma are dust mites, cockroaches and also bedbugs and fleas. Many other species that may infest a home may serve as a source of allegens such as Pharaoh ants.[21]
- Fungus spores (mold): fungus reproduce by releasing spores into the air, if the spores land in a good place form them to grow then a new fungus starts. Breathing in these spores can trigger asthma. One of the most common types of fungus spores found in both outside and outside environments are from a group (genus) known as aspergillus.
- Strong emotions such as anger, stress and even laughter may worsen asthma symptoms.
- Outdoor air pollution can come from many sources such as car and truck fumes in areas of heavy traffic and chemicals in the air near factories and refineries.
- Weather: changes in the weather can trigger an asthma attack. Changes in air temperature can trigger an attack not just cold air. If a person goes from being outside in the cold into a warm house the sudden change can cause a broncospasm. Sudden changes in humidity also plays a part.[22]
The best way to deal with asthma triggers is to learn what they are and avoid them if possible, and if not totally avoidable then adjust one's behavior to deal with them. Example: running on a cold winter day right up to the doorstep of a warm house and going immediately inside; the sudden temperature change can cause an attack and could have been avoided. In general but especially with a medical condition such as asthma it is necessary to be aware of one's environment and what's in it, both indoors and outdoors. Most often the Asthma is triggered by allergens. One big source of allergens is the carpet. Totally replace it with a tiles floor reduce the possibility to create a good environment for the allergens and it is more simple to clean and disinfect.
Asthma attack
An asthma attack is when, after a period of time when aperson has had only a few or no symptoms of asthma, the asthma gets worse all of a sudden, usually because of being exposed to one or more triggers. When the asthma attack happens, the tissue inside the airways swell because of inflammation - which is how the body tries to protect itself from harmful things, like germs and irritants. When the tissues swell the opening (called the lumen) in the airway gets very narrow.
The smooth muscles (which are the kind of muscles in the body that do not contract voluntarily, like the ones in the arm) around the bronchi and bronchioles begin to spasm or contract which makes the opening in the airway even narrower. This is called a bronchospasm.
Inside the lining of the airways are glands called, submucosal glands, and above them, closer to the opening in the airway are cells called goblet cells - because they are shaped kind of like a goblet, which is a type of cup. The submucosal glands and the goblet cells make mucous which helps protect the inside of the airways. The mucous in the airways of healthy lungs is a thin film which traps irritants such as dust particles and pollen so they do not damage the airways and keep them from entering the air sacs (alveoli).
There are tiny hairs lining the airway called cilia. The cilia wave back and forth like a liitle whips, and help push the mucous and the trapped particles up the airways to the "pharynx. From there the mucous, the trapped particles from the lower airways can be coughed up (this is called sputum).
During an asthma attack the submucosal glands and the goblet cells start making much more mucous than normal, and the mucous is also thicker than normal. This makes it very hard for the cilia to do their job, and bring the mucous up out of the airways. So now there is too much mucous being made, and not enough being brought up by the cilia. The airways are already to narrow to breathe properly because of the tissue swelling caused by inflammation and the constriction caused by the bronchospasms, so the extra mucous blocks the airway even more. This makes breathing very difficult. In fatal asthma attacks the airways can become so constricted and/or plugged with mucous that no air can get through at all.[23][24]
There are other signs of breathing difficulty as in an asthma attack, which are important to learn, and knowing them can help tell if someone who cannot talk is having breathing problems. People who may not be able to let somebody know they are having breathing problems include babies and young children.
Some of the other signs of asthma include:
- Chest and neck retractions; which cause muscles within the chest and neck not normally used too much when breathing, to begin contracting as they try and help to take in more air. Retractions are how the body tries to get enough air because of the difficulty in breathing normally because of the asthma attack. These retractions cause the skin of the chest wall, the skin of the neck and or the breastbone (sternum) to move in when breathing. There are different types of retractions which depend on which muscles start contracting, and this depends on how much difficulty a person is having breathing during an attack.[25]
- Nasal flaring is when the opening of the nostrils get larger than normal during breathing. It is often a sign that a person is having difficulty in breathing.
- Blue lips and fingertips: oxygen which is in the air we breathe, is what makes blood have a red color. Blood without oxygen has a blue color. Oxygen enters the body through the air sacs (alveoli) which are at the end of the airways. During an asthma attack it difficult for the body to get enough oxygen because it is difficult to get enough air. As less air with oxygen in it makes it to the air sacs and into the blood, there is less red blood (blood with oxygen in it) and more blue blood (blood without oxygen in it). The blue color of the lips and under the fingernails is because of the blue blood, which can be seen in the small blood vessels under the skin. More parts of the body start turning blue the longer the body goes without oxygen. When parts of the body turn blue because of lack of oxygen it is called cyanosis.
- Sweating : sweating may be noticed especially on the forehead, but the skin does not feel warm, it may feel cool and clammy to touch.
- Rapid breathing (tachypnea); breathing in and out much faster than normal.
- Rapid heart beat: (tachycardia): the heart starts beating much faster than normal.[26]
Diagnosis
A diagnosis of asthma is based on a person's:
- Medical history; information such as what signs and symptoms of asthma have they had
- Family medical history; has anyone they are related to had asthma or related conditions such as occur with those who are atopic
- Physical examination and testing
Diagnostic Tests
There is no specific test that can tell if a person has asthma, however there are tests that can help in the diagnosis when the results are considered along with the medical and family history and physical exam
- Lung function tests [Pulmonary function tests (PFTs)]
- Spirometry; measures how much air the lungs are able to breathe in and how much air they breathe out and how fast a person can exhale.
- Bronchoprovocation test; in this test the airways (bronchi and bronchioles) are provoked (to try and make something happen) into having a bronchospasm (make the airways constrict) this is to see how sensitive they are. Some of the things done to provoke a bronchospasm are making the person exercise, breathing cold air that gets colder, or breathing in a special chemical called methacholine. The results of bronchoprovocation are checked using spirometry.
- Spirometry; measures how much air the lungs are able to breathe in and how much air they breathe out and how fast a person can exhale.
Differential diagnoses
Differential diagnoses are different medical disorders which may cause the same symptoms. Before a doctor makes a final diagnosis, which means they are sure of what medical disorder is causing the problem, they think of what other medical conditions have the same or almost the same symptoms, and make sure it's not one of them.[27]
The differential diagnoses of asthma include:
- Bronchiectasis
- Chronic obstructive pulmonary disease (COPD)
Airway remodeling
Airway remodeling is when there are permanent physical changes to the airways that also affects how they work. This may happen after chronic long-term asthma. After cycles of inflammation, damage and repair to the airways. permanent remodeling of the airways may occur. This is when the physical structure of the airway changes. This will cause permanent airway narrowing (they are always more narrow than normal and get narrower during an asthma attack), bronchospasms are more easily triggered (bronchial hyperresponsivenes), airway edema (fluid in the airway), and mucus hypersecretion (too much mucous is made) as well as the build-up of collagen around the airway which is called fibrosis. Airway remodeling has been observed in chldren as young as six.[28]
Not managing asthma properly can lead to airway remodeling and this can increase the risk of dying from an asthma attack.[29][30] One of the main problems which cause poor asthma management is not using the asthma inhaler correctly.[31] One of the main reasons for improper inhaler use is the asthma patient not having the proper knowledge in using the inhaler due to not receiving proper instruction.[32]
Goblet cell and submucosal gland hyperplasia: Among the physical changes that may happen in airway remodeling is goblet cell hyperplasia and submucosla gland hyperplasia. Submucosal glands and goblet cells make mucous which helps to protect the airways by trapping harmful particles like dust and pollen. The mucous is normally a thin film which lines the airways. The mucous and whatever particles they trap are brought up to the pharynx by tiny (microscopic) hairs on the inside of the airway that move back and forth called cilia.
During an asthma attack the submucosal glands and goblet cells make too much mucous, and it is thicker than normal which makes it harder for the cilia to bring the mucous up. When airway remodeling happens the body may make many more submucosal glands and goblet cells than normal, which means even more mucous is made. There may be too much mucous for the cilia to bring up and the airway may become blocked. This is one of the reasons that people with airway remodeling often have more severe asthma. In fatal cases the airway may have become totally plugged causing asphyxia.[33]
Airway Reconstruction Methods
Regular Breastfeeding sessions are a proven benefit to airway reconstruction. While previous studies have shown a similar effect between breastfeeding and asthma risk, this research is the first that showed a link between the length of breastfeeding and the number of wheezing episodes. Also, this study found evidence that the first asthma-related symptoms occur earlier in life if children were breastfed for shorter lengths of time or not exclusively. The study shows it’s not the nutritional benefit from the liquid, it’s the pull on lung of which dilates the smooth muscles of the air passage. Dry-nursing has actually proven to had been more beneficial in this study for strengthening airway health in both children and adults. Dilating the airways will strengthen them and the lungs themselves.
Treatment
A woman using a metered-dose asthma inhaler (or just inhaler for short), which has medicine to treat an asthma attack inside. When the inhaler is put in the mouth and pressed, the medicine is sprayed into the throat and then enters the lungs.[34]
An asthma action plan or management plan, is used to help a person with their asthma. It shows what kind of medicines to take, and when to take them. How to take care of their asthma everyday, AND how to take care of their asthma when it gets worse, or when they have an asthma attack. It helps them know when it is time to call the doctor or go to the emergency room.[35]
Asthma can be controlled most often by avoiding contact with triggers and by using certain drugs. Most asthma sufferers carry special medicines around with them. These are called inhalers. The medicine inside the inhaler opens the tubes that go to the lungs. The inhaler is usually used to prevent an asthma attack, or to stop an attack that is already happening.
Rescue medicine — A rescue medicine is an inhaler ("puffer") that is used if a person thinks they are having an asthma attack.
Controller medicine — A controller medicine is a medicine in either a pill or an inhaler taken every day to prevent asthma attacks.
Common treatment in a hospital
Hospitals have other options they can use in an emergency when the regular treatments don't work:
- Oxygen
- Certain drugs that act like an asthma spray, but are much stronger
- Certain drugs that can be given through an IV (intravenously).
- Steroids
- Breathing aids (including tubes, and valves in very severe cases)
Unconventional Treatments / At Home Remedies
- Warm steam baths have often been used to help alleviate nasal congestion and airway irritation associated with asthma.
- Omega-3 fatty acids are often used as a natural remedy to help prevent and treat heart disease. Though some research suggests that omega-3s may also help to decrease airway inflammation and boost lung function
- The Buteyko Breathing Technique is based on the premise that raising blood levels of carbon dioxide through shallow breathing can help people with asthma. Carbon dioxide is believed to dilate the smooth muscles of the airways.
- Hot beverages are known to open breathing passages, have been said to open airways for irritated asthma symptoms. This method has been said to give temporary relief.
- High consumption of apples may protect against asthma. Daily intake of fruits and vegetables in childhood decreased the risk of asthma.
- Breastfeeding or the reflection of in adolescence and adults has been proven to strengthen and promote airway health. The strain from the pull on the lung will dilate the smooth muscles of the airways. Extended therapeutic sessions on a regular basis have been shown to dramatically improve air passage function, and promote less asthma complications.
Drugs that may worsen an asthma attack
There are certain types of drugs that make asthma worse or that can trigger such an attack. Certain types of drugs should only be used in very specific situations. Some of these drugs are:
- Non-steroidal anti-inflammatory drugs or 'NSAID' for short. Aspirin is a NSAID and some people are allergic to it, or may have a higher risk of becoming allergic to it, even if they had used it before.
- Beta blockers are a kind of drug used to treat heart problems, but should not be taken by people with asthma.
- Acetaminophen is another drug that is believed might help not only to cause asthma, but also make asthma worse in people who already have it. Acetaminophen is an analgesic, a pain reliever. Because of its pain-reliving properties, Acetaminophen is often added to other drugs. Labels should always be read when taking any kind of medicine, including over-the-counter drugs.[36]
- ACE Inhibitors; are a type of drug usually used to treat high blood pressure and heart disease. They usually don’t make asthma worse, but in rare cases they may cause some of the signs and symptoms of asthma, such as airway obstruction and coughing, especially in the first few weeks of taking ACE Inhibitors.[37][38]
- Sleeping pills and trainquilizers; should usually not be taken by people with asthma.[39]
Managing comorbid asthma, depression and/or anxiety
Depression and anxiety have a negative impact on asthma.[40] Comorbid anxiety with asthma is particularly confusing because of the similarity of symptoms and interference in perception and treatment of asthma. The National Asthma Council Australia [41] recommends treatment for comorbid psychological symptoms. Cognitive Behaviour Therapy (CBT) is one recommended treatment for anxiety [42] and depression.[43] There is tentative research evidence suggesting that a program of CBT amended for asthma, delivered in conjunction with medical treatment and in close liaison with your medical team, can improve anxiety, asthma and quality of life.[40] Clinicians intending to deliver CBT for comorbid asthma, anxiety or depression should refer to [44] and the research reviewed by [40] for guidance on safe and effective intervention.
The Global Initiative for Asthma
The global Initiative for Asthma (GINA), launched in 1993, is a collaborative effort between the World Health Organisation (WHO), the National Institutes of Health USA (NIH), and the National Heart, Lung and Blood Institute. Its aims include; to increase public awareness of asthma, encourage research into the causes for the increasing prevalence of asthma worldwide, encourage research into the links between asthma and environmental factors, improve the effectiveness of asthma management practices, reduce the mortality and morbidity rates associated with asthma, and make treatments for asthma more readily available.
One of the ways in which GINA fulfils these aims is by producing medical guidelines on the management of asthma, which based on a systematically conducted review of the most recent-worldwide literature. These guidelines are free and available to all patients and clinicians from the GINA website. The GINA main report is updated annually and aims to reflect evolving best practice as it highlights changes in asthma management strategies.
GINA established ‘World Asthma Day’ in 1998, with the first event organised in Barcelona, Spain. It is held annually on the first Tuesday of May, and includes the participation of more than 35 countries.[45]
Comorbidities
Often, having one medical problem makes it more likely a person will also have one or more other medical or psychiatric problems. These other disorders are the "comorbid problems" or "comorbidities".[46] There are various comorbid medical and psychiatric conditions associated with asthma.
Respiratory disorders
- Chronic obstructive pulmonary disorder (COPD)
- Respiratory infections
- Chronic sinusitis[47]
- Rhinitis: allergic (atopic), nonallergic
- Hyperventilation syndrome[48]
- Allergic bronchopulmonary aspergillosis (ABPA) is a disorder that affects the airways of the lungs which is caused by an allergic hypersensitivity to the fungus Aspergillus fumigatus.
Gastrointestinal disorders
- Gastroesophageal reflux disease (GERD)
- Eosinophilic esophagitis (EE)
Psychiatric disorders
- Depression
- Anxiety disorders
- Panic disorder
Sleep disorders
- Obstructive sleep apnea
Skin disorders
- Atopic dermatitis (AD): is a type of eczema
Epidemiology
>10.1 7.6-10.0 5.1—7.5 2.5-5.0 0-2.5 no data: for these areas there was not enough information. |
In medicine epidemiology is the study of what causes diseases and medical conditions, how often they happen, where they happen and who they happen to.[50]
It is more common in developed countries than developing countries. The United States and Canada have some of the highest asthma rates in the world even though they are not poor countries. In Africa the country of South Africa has the highest asthma rate on the whole continent even though it is one of the richest countries.
More than 80% of the people who die from asthma are usually from low and middle income countries, but not always, as South Africa has the fourth highest death rate in the world even though it is one of the richer countries in the world.[51] In the United States the death rates are higher for females, adults and people of African descent.[52]
As of 2011, 235–300 million people worldwide are affected by asthma,[53] and approximately 250,000 people die per year from the disease. Rates vary between countries with prevalences between 1 and 18%.
The amount of asthma cases reported each year has gotten much higher between the 1960s and 2008[54][55][56] Rates of asthma have plateaued in the developed world since the mid-1990s with recent increases primarily in the developing world.[57] Asthma affects approximately 7% of the population of the United States and 5% of people in the United Kingdom.[58] Canada, Australia and New Zealand have rates of about 14–15%.[59]
Other websites
References
- ↑ Smith, Terry L. (2009). Asthma. Infobase Publishing. p. 46. ISBN 0-7910-9663-7.
- ↑ Yang IV, Schwartz DA. Epigenetic mechanisms and the development of asthma. J Allergy Clin Immunol. 2012 Dec;130(6):1243-55. PMID 23026498
- ↑ Crystal-Peters J, Neslusan C, Crown WH, Torres A. Treating allergic rhinitis in patients with comorbid asthma: the risk of asthma-related hospitalizations and emergency department visits. J Allergy Clin Immunol. 2002 Jan;109(1):57-62. PMID 11799366
- ↑ Paul, William E. (2008). Fundamental Immunology. Lippincott Williams & Wilkins. ISBN 978-0-7817-6519-0.
- ↑ Thurlbeck, William M.; Churg, Andrew (1995). Pathology of the Lung. Thieme. p. 144. ISBN 978-0-86577-534-3.
- ↑ Beasley RW, Clayton TO, Crane J, et al, ISAAC Phase Three Study Group. Acetaminophen use and risk of asthma, rhinoconjunctivitis, and eczema in adolescents: International Study of Asthma and Allergies in Childhood Phase Three. Am J Respir Crit Care Med. 2011 Jan 15;183(2):171-8. Acetaminophen use and risk of asthma, rhinoconjunctivitis, and eczema in adolescents: International Study of Asthma and Allergies in Childhood Phase Three. PMID 20709817
- ↑ International Study of Asthma and Allergies in Childhood: ISAAC Phase Three
- ↑ Gresele, Paolo (2002). Platelets in Thrombotic and Non-Thrombotic Disorders: Pathophysiology, Pharmacology and Therapeutics. Cambridge University Press. p. 861. ISBN 978-0-521-80261-1.
- ↑ American College of Physicians: Internal medicine updates ACP Press pp.239-240. 2003
- ↑ McBride JT. Pediatrics. The association of acetaminophen and asthma prevalence and severity. 2011 Dec;128(6):1181-5. PMID 22065272
- ↑ White, Lois; Duncan, Gena (2002). Medical-surgical Nursing: An Integrated Approach. Taylor & Francis. p. 385. ISBN 978-0-7668-2566-6.
- ↑ posterior view: Merriam-Webster: Visual Dictionary Online
- ↑ Juzar Ali, Warren Summer, Michael Levitzky: Pulmonary Pathophysiology, A Clinical Approach: McGraw-Hill Medical; 3 edition, 2009 p.25 ISBN 978-0-07-161154-1
- ↑ Brent, Jeffrey (2005). Critical Care Toxicology: Diagnosis and Management of the Critically Poisoned Patient. Gulf Professional Publishing. p. 1000. ISBN 978-0-8151-4387-1.
- ↑ Severe Asthma: Pathogenesis and Clinical Management (Lung Biology in Health and Disease): editors: Stanley J Szefler, Donald Y. M. Leung. CRC Press; 2 edition (2001); p.382 ISBN 978-0-8247-0552-7
- ↑ Sullivan, John Burke; Krieger, Gary R. (2001). Clinical Environmental Health and Toxic Exposures. Lippincott Williams & Wilkins. p. 230. ISBN 978-0-683-08027-8.
- ↑ Tan KS. Premenstrual asthma: epidemiology, pathogenesis and treatment. Drugs. 2001;61(14):2079-86. PMID 11735634
- ↑ Fritz, Marc A.; Speroff, Leon (2011). Clinical Gynecologic Endocrinology and Infertility. Lippincott Williams & Wilkins. p. 588. ISBN 0-7817-7968-5.
- ↑ Dolinak, David; Matshes, Evan W.; Lew, Emma O. (2005). Forensic Pathology: Principles and Practice. Academic Press. p. 356. ISBN 978-0-12-219951-6.
- ↑ Rosenthal LA, Avila PC, Heymann PW, et. al. Viral respiratory tract infections and asthma: the course ahead. J Allergy Clin Immunol. 2010 Jun;125(6):1212-7. doi: 10.1016/j.jaci.2010.04.002. PMID 20513518
- ↑ Kim CW, Kim DI, Choi SY, et al. Pharaoh ant (Monomorium pharaonis): newly identified important inhalant allergens in bronchial asthma. J Korean Med Sci. 2005 Jun;20(3):390-6. PMID 15953858
- ↑ Porth, Carol (2011). Essentials of Pathophysiology: Concepts of Altered Health States. Lippincott Williams & Wilkins. p. 576. ISBN 1-58255-724-1.
- ↑ Green FH, Williams DJ, James A, et al. Increased myoepithelial cells of bronchial submucosal glands in fatal asthma. Thorax. 2010 Jan;65(1):32-8. PMID 19996346
- ↑ Carroll NG, Mutavdzic S, James AL. Increased mast cells and neutrophils in submucosal mucous glands and mucus plugging in patients with asthma. Thorax. 2002 Aug;57(8):677-82. PMID 12149526
- ↑ Fleisher, Gary R.; Ludwig, Stephen (2010). Textbook of Pediatric Emergency Medicine. Lippincott Williams & Wilkins. p. 651. ISBN 1-60547-159-3.
- ↑ Rahm, Stephen J. (2005). Pediatric Case Studies for the Paramedic. Jones & Bartlett Learning. p. 6. ISBN 978-0-7637-2582-2.
- ↑ "Differential diagnosis". Free Merriam-Webster Dictionary. 2012. Retrieved December 19, 2012.
- ↑ Wheeler, Derek S.; Wong, Hector R. (2007). Pediatric Critical Care Medicine: Basic Science And Clinical Evidence. Springer Science & Business Media. p. 46. ISBN 978-1-84628-463-2.
- ↑ A.L. James, J.G. Elliot, M.J. Abramson, E.H. Walters Time to death, airway wall inflammation and remodeling in fatal asthma. Eur Respir J 2005; 26: 429–434. ERS Journals Ltd 2005
- ↑ Therapeutic Targets in Airway Inflammation Eds. N. Tony Eissa, David P. Huston : CRC Press; 1 edition (2003) pp.752-753. ISBN 978-0-8247-0956-3
- ↑ Al-Jahdali H1, Ahmed A, Al-Harbi A, Khan M, Baharoon S, Bin Salih, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma Clin Immunol. 2013 Mar 6 ;9(1):8. doi: 10.1186/1710-1492-9-8.
- ↑ Al-Jahdali H, Anwar A, Al-Harbi A, Baharoon S, Halwani R,et al. Factors associated with patient visits to the emergency department for asthma therapy. BMC Pulm Med. 2012 Dec 17; 12:80.PMID 15334198
- ↑ Barnes, Peter J.; Drazen, Jeffrey M.; Rennard, Stephen I. (2009). Asthma and COPD: Basic Mechanisms and Clinical Management. Academic Press. p. 217. ISBN 0-12-374001-0.
- ↑ Falvo, Donna R. (2005). Medical and Psychosocial Aspects of Chronic Illness and Disability. Jones & Bartlett Learning. p. 338. ISBN 978-0-7637-3166-3.
- ↑ Douglas, J Graham; Elward, Kurtis S (2010). Asthma: Clinician's Desk Reference. CRC Press. p. 100. ISBN 978-1-84076-082-8.
- ↑ Nursing Nonprescription Drug Handbook. Lippincott Williams & Wilkins. 2001. p. 390. ISBN 978-1-58255-101-2.
- ↑ Lunde H, Hedner T, Samuelsson O, et al. Dyspnoea, asthma, and bronchospasm in relation to treatment with angiotensin converting enzyme inhibitors. BMJ. 1994 Jan 1;308(6920):18-21. PMID 8298346
- ↑ Gershwin, M. Eric; Albertson, Timothy; Albertson, Timothy Eugene (2001). Bronchial Asthma: Principles of Diagnosis and Treatment. Springer Science & Business Media. p. 364. ISBN 978-0-89603-861-5.
- ↑ Ayd, Frank J. (2000). Lexicon of Psychiatry, Neurology, and the Neurosciences. Lippincott Williams & Wilkins. p. 675. ISBN 978-0-7817-2468-5.
- ↑ 40.0 40.1 40.2 Kew, K., Nashed, M., Dulay, V., Yorke, J. (2016) Cognitive behavioural therapy (CBT) for adults andadolescents with asthma. Cochrane Database of Systematic Reviews 2016, Issue 9.
- ↑ Australian Asthma Handbook – Quick Reference Guide, Version 1.1. (2015) National Asthma Council Australia. http://www.asthmahandbook.org.au
- ↑ NICE (2011). National Institute for Health and Care Excellence. Generalised anxiety disorder and panic disorder (with or without agoraphobia) in adults: management in primary, secondary and community care. NICE guidelines [CG113]. Published date: January 2011. www.nice.org.uk/guidance/cg113
- ↑ NICE (2009). National Institute for Health and Care Excellence. Depression in adults: the treatment and management of depression in adults. NICE guidelines [CG90]. Published date: October 2009. www.nice.org.uk/guidance/cg90
- ↑ Feldman, J., Giardino, N., & Lehrer, P. (2000). Asthma and panic disorder. In D. Mostofsky and D. Barlow (Eds). The management of stress and anxiety in medical disorders (pp. 220 -239). Needham Heights, MA:Allyn & Bacon.
- ↑ "About Us - Global Initiative for Asthma". Global Initiative for Asthma - GINA. Retrieved 2019-12-09.
- ↑ Comorbid | Definition of Comorbid by Merriam-Webster: Free Merriam Webster Dictionary, 2012. Retreived February 25, 2013
- ↑ Wilmott, Robert W.; Kendig, Edwin L.; Boat, Thomas F.; Bush, Andrew; Chernick, Victor (2012). Kendig and Chernick's Disorders of the Respiratory Tract in Children. Elsevier Health Sciences. ISBN 1-4377-1984-8.
- ↑ Fleisher, Gary R.; Ludwig, Stephen (2010). Textbook of Pediatric Emergency Medicine. Lippincott Williams & Wilkins. p. 1652. ISBN 1-60547-159-3.
- ↑ Global Initiative for Asthma[dead link]
- ↑ epidemiology: Free Merriam Webster Dictionary 2013, retrieved January 11, 2013
- ↑ World Health Organization. "WHO: Asthma". Archived from the original on 15 December 2007. Retrieved 2007-12-29.
- ↑ Centers for Disease Control and Prevention: NCHS Data Brief Number 94, May 2012; Trends in Asthma Prevalence, Health Care Use, and Mortality in the United States, 2001–2010. retrieved on March 3, 2013 Products - Data Briefs - Number 94 - May 2012
- ↑ "World Health Organization Fact Sheet Fact sheet No 307: Asthma". 2011. Archived from the original on 2011-06-29. Retrieved February 20 17th,2013.
{{cite web}}: Check date values in:|accessdate=(help) - ↑ Grant EN, Wagner R, Weiss KB (August 1999). "Observations on emerging patterns of asthma in our society". J Allergy Clin Immunol. 104 (2 Pt 2): S1–S9. doi:10.1016/S0091-6749(99)70268-X. PMID 10452783.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Anandan C, Nurmatov U, van Schayck OC, Sheikh A (February 2010). "Is the prevalence of asthma declining? Systematic review of epidemiological studies". Allergy. 65 (2): 152–67. doi:10.1111/j.1398-9995.2009.02244.x. PMID 19912154.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Mason, John F. Murray (2010). Murray and Nadel's textbook of respiratory medicine (5th ed. ed.). Philadelphia, PA: Saunders/Elsevier. pp. Chapter 38. ISBN 978-1-4160-4710-0.
{{cite book}}:|edition=has extra text (help) - ↑ Bousquet, J (2005 Jul). "The public health implications of asthma". Bulletin of the World Health Organization. 83 (7): 548–54. PMID 16175830.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Anderson, HR; Gupta R; Strachan DP; Limb ES (January 2007). "50 years of asthma: UK trends from 1955 to 2004". Thorax. 62 (1): 85–90. doi:10.1136/thx.2006.066407. PMC 2111282. PMID 17189533.
- ↑ Masoli, Matthew (2004). Global Burden of Asthma (PDF). p. 9. Archived from the original (PDF) on 2013-05-02. Retrieved 2013-02-20.