Exsanguination
Exsanguination is losing enough blood to cause death. A person does not have to lose all of their blood to exsanguinate. People can die from losing half to two-thirds of their blood.[1]
The average adult has about 4 to 6 liters of blood (9 to 12 US pints) in their body. The average man has more blood than the average woman, and people who weigh more or are taller than others have more blood.[1] This means a person can die from losing 2 1/2 to 4 liters of blood. To compare, this is five to eight times as much blood as people usually give in a blood donation.[2]
Children and babies have much less blood than adults, and can exsanguinate by losing much less blood than adults.[3]
Exsanguination is often called bleeding to death or bleeding out. It is a medical emergency.
Definition
Doctors define exsanguination this way:[4]
- The patient has lost over 40% of their blood (2 to 2.4 liters in an average adult)
- The patient is still losing blood
- The bleeding is so bad that if it is not stopped quickly, the patient will die
Types of bleeding
Bleeding can be external or internal.[1]
"External" means "outside the body." External bleeding is visible - it can be seen outside the body. For example, a person who cuts their hand and has blood on their hand is having external bleeding.
"Internal" means "inside the body." Internal bleeding cannot be seen, because it is inside the body. For example, a person who is bleeding into their brain because of a stroke is having internal bleeding.
Sometimes, bleeding can be both internal and external. A person can exsanguinate from internal bleeding, external bleeding, or both.[5]
Causes
Exsanguination is usually caused by major blood vessels getting injured or breaking open. Smaller blood vessels bleed less, and bleed slower, so it is harder to exsanguinate if they are injured.[1]
Injuries
Exsanguination can be caused by trauma (injuries). Out of all people who die from injuries, 30-40% die from exsanguination.[6] Up to half of these people (33-56%) die before they even get to the hospital.[6]
Penetrating trauma (an injury where something breaks the skin) is one of the most common causes of exsanguination.[7] This is especially true for gunshot wounds to places like the heart, chest, or head, which all have major blood vessels in them.[6][7]
Other injuries that can cause exsanguination include:[6]
- Injuries which cut major arteries, like the aorta, carotid artery (in the neck), or femoral artery (in the groin and legs)
- Motor vehicle accidents
- Amputation of an arm or leg
A person can exsanguinate from internal bleeding if:[3][6]
- They are bleeding into their chest or abdomen (for example, because of blunt force trauma)
- They break their pelvis
- They break both of their femurs (thigh bones)
Exsanguination is one of the most common causes of death in soldiers at war.[8][9] It is usually caused by gunshot wounds, motor vehicle accidents, or explosions.[8][9]
Medical problems
Some medical problems can make a person exsanguinate by bleeding internally. These problems include:[3][5]
- An aneurysm in the aorta that breaks. This can cause a person to exsanguinate in just a few minutes.
- Sepsis, which can cause the infection to eat away at the walls of the blood vessels. Eventually the walls break and the blood vessels start to bleed.
- Bleeding after childbirth. Around the world, one woman dies every two minutes from exsanguination after childbirth. Most of these deaths happen in developing countries.[10]
- Bleeding from the spleen, liver, or intestines
- A very bad peptic ulcer
- A tumor that eats into a major blood vessel, like a tumor in the neck that eats into the carotid artery and makes it start bleeding
Effects
If a person is losing blood very quickly (for example, from a broken aortic aneurysm), they will only be conscious for 20 seconds to a few minutes.[5] If blood loss is slower, and the person does not get medical treatment, they may be conscious for a few hours. However, they will get more and more confused and tired as they lose more blood. Eventually the person will go into a coma because there is not enough blood left in their body to bring oxygen to their brain. Finally their heart will stop and they will die.[5]
Exsanguination is a syndrome
Doctors call exsanguination a syndrome (a group of symptoms), because it causes so many problems in the body.[7]
Hypothermia
Blood helps keep us warm. Because of this, losing a lot of blood causes hypothermia.[5]
Coagulopathy
Coagulopathy means that the blood no longer clots normally.[11] When a person loses blood, they also lose the platelets and blood-clotting proteins the blood carried. These platelets and proteins make the blood clot.[12] If a person loses too much blood, they will not have enough platelets or proteins left to make the blood clot.
Acidosis
Acidosis means that the body makes too much acid.[1] Usually, the body makes energy out of oxygen (carried in blood) and glucose (sugar). (This is called aerobic respiration.)[13] If a person loses a lot of blood, there will not be enough oxygen in the blood that is left to make energy this way. The body switches to anaerobic respiration, and makes energy out of glucose without needing oxygen. However, this creates many acidic waste products (chemicals that the body does not need, which are left over after the body does chemical reactions).[13] Eventually these waste products can build up so much that they poison the body. This is called acidosis.[3]
Arrhythmia
When the heart does not get enough blood, it can start beating in ways that are not normal.[3] When this happens because of exsanguination, it usually means that the patient is close to dying.[6]
Shock
If a person loses enough blood, they will go into shock.[1] This means the body's most important organs are not getting the blood, oxygen, and nutrients they need to survive. It also means that the body is not able to get rid of waste products, like acids. If shock gets bad enough, it will kill the person.[3]
Treatment
First aid
First aid is an important first step in treating exsanguination. Things that regular people can do to help include:[14]
- Calling 9-1-1 or another local emergency telephone number immediately
- Trying to stop the bleeding by:
- Pressing against the place that is bleeding
- If the person is bleeding from an arm or leg, lifting the arm or leg above the level of the person's heart
- Making a tourniquet and wrapping it tightly above where the person is bleeding
- Lying the person down, and raising their legs if possible
- If the person is coughing or vomiting blood, turning them on their side so they do not choke
- Keeping the person warm
- Trying to help the person stay calm
If possible, a person giving first aid should wear gloves any time they touch another person's blood. The sick or injured person may have an infection that can be spread through blood, like HIV or hepatitis. Wearing gloves will protect the person giving first aid from getting these infections.[14]
First aid saved many lives during the Boston Marathon bombings, when ordinary people used belts for tourniquets or used their own hands to press against bleeding wounds.[15] The three people who died in the bombings died right away.[15] There were many other people who were hurt badly enough that they could have exsanguinated. For example, some people's legs were blown off by the bombs. However, because of the help of ordinary people giving first aid (and because of emergency medical services), everyone who did not die right away survived.[15]
Emergency medical treatments
Emergency medical treatments for exsanguination include:[6]
- Tests, like ultrasounds or CT scans, to find the cause of bleeding if it is internal
- Surgery to fix the cause of the bleeding
- Treatments to warm the body up
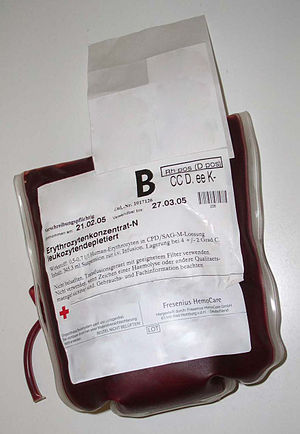
- Blood transfusions
- Giving fluids, like saline, through a needle into a vein to add to the amount of fluid that is in the person's body
- Giving medications to decrease acidosis
Risk factors
Risk factors for exsanguination
There are some risk factors which make a person more likely to exsanguinate. A few examples are:
- Being on anticoagulants (blood-thinning medications). These can make even a small wound bleed dangerously.[12]
- Having a blood clotting disorder, like hemophilia[3]
- Alcoholism. Drinking too much alcohol can damage the liver. If the liver is damaged, it cannot make blood-clotting proteins (like fibrinogen) as well as a healthy liver does.[16] This makes alcoholics more likely to bleed dangerously if they get hurt. Liver damage can also lead to a problem called esophageal varices, which can cause a person to exsanguinate by throwing up blood.[16]
- Advanced cancer. Of everyone who has advanced cancer and is not getting treated for their cancer, up to one in 10 people have dangerous bleeding.[5]
Risk factors for death from exsanguination
When a person is exsanguinating, they are more likely to die if:[7][17]
- They do not get into surgery quickly enough
- They have hypothermia, with a temperature under 34° C (93.2° F)
- Their blood is more acidic because of acidosis
- They needed to be given more than 4 liters of blood, or over 10 liters of fluids, to replace the blood they lost
- They lost more than 15 mL of blood per minute (losing blood this fast, the person would exsanguinate in less than 30–40 minutes)
- They have lower numbers of platelets when they first get to the hospital
- They are elderly
Related pages
- Blood
- Bleeding
- Arterial bleeding (one of the most dangerous kinds of bleeding)
- Blood clotting (also called "coagulation")
- Blood vessels
- Blunt force trauma
- Aneurysm
- Platelets
- Fibrinogen (a blood-clotting protein made in the liver)
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Mistovich, Joseph J.; Karren, Keith J.; Hafen, Brent (July 18, 2013). Prehospital Emergency Care (10th ed.). Prentice Hall. ISBN 978-0133369137.
- ↑ "Blood donation: What you can expect". Mayo Clinic. May 30, 2014. Retrieved February 16, 2016.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Sanders, Mick J.; McKenna, Kim D.;; et al. (2011). Mosby’s Paramedic Textbook. Jones & Bartlett Publishers. ISBN 9780323072755.
{{cite book}}: CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ↑ Asensio JA; Petrone P;. "Managing exsanguination: What we know about damage control/bailout is not enough". Baylor University Medical Center Proceedings. Baylor University Medical Center. 16 (3): 294–296. Retrieved February 16, 2016.
{{cite journal}}: Invalid|display-authors=etal 2003(help); Unknown parameter|pmcid=ignored (|pmc=suggested) (help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ↑ 5.0 5.1 5.2 5.3 5.4 5.5 "Hospice Palliative Care Program: Symptom Guidelines – Exsanguination" (PDF). Fraser Health. Hospice Palliative Care, Clinical Practice Committee, Fraser Health. November 24, 2006. Retrieved February 16, 2016.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Geeraedts LMG; Kaasjager HAH;. "Exsanguination in Trauma: A Review of Diagnostics and Treatment Options". Injury. Elsevier. 40 (1): 11–20. doi:10.1016/j.injury.2008.10.007. Retrieved February 16, 2016.
{{cite journal}}: Invalid|display-authors=etal 2009(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ↑ 7.0 7.1 7.2 7.3 Asensio JA; McDuffie L;. "Reliable Variables in the Exsanguinated Patient Which Indicate Damage Control and Predict Outcome". American Journal of Surgery. 182 (6): 743–751. PMID 11839351.
{{cite journal}}:|access-date=requires|url=(help); Invalid|display-authors=etal 2001(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ↑ 8.0 8.1 Pannell D; Brisebois R;. "Causes of Death in Canadian Forces Members Deployed to Afghanistan and Implications on Tactical Combat Casualty Care Provision". Journal of Trauma – Injury Infection & Critical Care. Lippincott Williams & Wilkins, Inc. 71 (5): S401-7. doi:10.1097/TA.0b013e318232e53f.
{{cite journal}}:|access-date=requires|url=(help); Invalid|display-authors=etal 2011(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ↑ 9.0 9.1 Holcomb JB; McMullin NR;. "Causes of Death in U.S. Special Operations Forces in the Global War on Terrorism: 2001-2004". Annals of Surgery. Lippincott Williams & Wilkins, Inc. 245 (6): 986–991. doi:10.1097/01.sla.0000259433.03754.98.
{{cite journal}}:|access-date=requires|url=(help); Invalid|display-authors=etal 2007(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ↑ "Maternal Health". United Nations Population Fund. United Nations. Retrieved February 16, 2016.
- ↑ Hunt, Beverley J. (2014). "Bleeding and Coagulopathies in Critical Care". New England Journal of Medicine. 370 (9): 847–859. doi:10.1056/NEJMra1208626. ISSN 0028-4793.
- ↑ 12.0 12.1 Shaph DR; Bouillon B;. "Management of Bleeding and Coagulopathy Following Major Trauma: An Updated European Guideline". Critical Care. 17 (2): R76. doi:10.1186/cc12685. PMC 4056078. PMID 23601765.
{{cite journal}}: Invalid|display-authors=etal 2013(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ↑ 13.0 13.1 "Respiration". Chemistry for Biologists. Royal Society of Chemistry. 2004. Retrieved February 16, 2016.
- ↑ 14.0 14.1 "Severe Bleeding: First Aid". Mayo Clinic. Mayo Foundation for Medical Education and Research. October 21, 2014. Retrieved February 16, 2016.
- ↑ 15.0 15.1 15.2 Biddinger, PD; Baggish, A;. "Be Prepared – The Boston Marathon and Mass-Casualty Events". New England Journal of Medicine. 368: 1958–1960. doi:10.1056/NEJMp1305480.
{{cite journal}}:|access-date=requires|url=(help); Invalid|display-authors=etal 2013(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ↑ 16.0 16.1 Tsokos M; Turk EE 2002. "Esophageal Variceal Hemorrhage Presenting as Sudden Death in Outpatients". Archives of Pathology and Laboratory Medicine. College of American Pathologists. 126 (10): 1197–1200. PMID 12296758.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ↑ Zhang WB; Wang WY;. "Risk Factors of Mortality in Non-Trauma Exsanguinating Patients that Require Damage Control Laparotomy". ANZ Journal of Surgery. Royal Australasian College of Surgeons. 80 (4): 258–64. doi:10.1111/j.1445-2197.2009.05087.x. PMID 20575953.
{{cite journal}}:|access-date=requires|url=(help); Invalid|display-authors=etal 2010(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link)